Medicine field and healthcare are expected to be largely influenced by Artificial intelligence (A.I.) in the near future. The application could vary from deploying medicines using AI-powered biotech, investigating patterns and impact of diseases/pandemic (e.g. Corona-Virus), identifying side effects from various drugs and/or combination of drugs, AI-based clinical validation, etc.
This idea may still be in its infancy; however, every year different findings or studies are being shared around this. There appears to be a positive path for A.I. indicating that medicinal practices and field might get benefited. It is important that experts, practitioners, surgeons, scientists and technologists, etc. all come together to support, enhance and lead in this process.
We are going to share some of the examples of the use of AI in medicine in coming forthcoming posts.
Use of AI in medicine and healthcare again came into a discussion this year when the FDA approved a software programme that allows medical professionals to perform cardiac ultrasound imaging without specialized training.
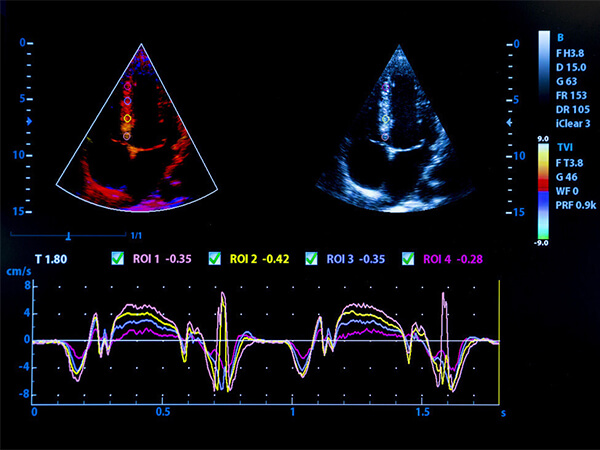
In this programme, A.I. provides real-time guidance and also the ability to save images of diagnostic quality – this assists those performing an ultrasound scan. (the AI is expected to emulate the guidance from an expert sonographer).
The success of A.I. in medicine and healthcare will depend on how it can prove itself in comparison to practice-based and evidence-based medicinal or clinical practices. There is probably a need to build processes, policies. Naturally, as the field deals with life and death of a living being, there will be questions, suspicions and probably reluctance to use it in a first go. Unless we all are assured – we can not believe that it will become a mainstream practice in this field.
Also Read: Is Artificial Intelligence a Future Threat to Mankind?
A considerable percentage of patients across the globe struggle with mental health issues, but the treatment is difficult to access (compared to other treatments) and maybe slightly more expensive to use regularly.
In the case of mental and behavioural healthcare, requires a different approach in connecting patients with facilities and services. AI-driven applications/programs could be a great contributor to the answer.

These days we see a number of smartphone-based apps around areas like behavioural therapy, sleep disorders, integrated group therapy, etc. The trend has started and is showing promise for treating conditions such as depression, disorders, substance abuse, etc.
There are some applications that might be made available in commercial interest without being rigorously validated or tested. Various research institutions/organizations are also developing AI-based tools/apps with clinical trials and these are showing good results.
Stakeholders involved in these initiatives must also give due importance to patient privacy/security when considering AI implementation. One of the most important aspects to consider is – a human touch or the practitioner-patient relationship. After all, even today, convincing words / caring remarks or even a simple smile from the practitioner brings in a lot of comfort to the patient. And hence, it must not be forgotten that patients still want to talk to their practitioners & AI should not replace this interaction.
Maybe the start is in assisting programs or probably the areas where – the ultimate decision could be made on the basis of AI and evidence from tests, reports, parameters collated by the field expert.

The pace at which the demand for considering AI in medicine and healthcare would increase, the same pace would be required to build implementation framework, policies, fall-back processes, even psychological assistance to patients, etc.
Ultimately, we would not want the technology to be available and waiting for the right process or framework to be in place and the most important aspect is – someone still needs to be in charge of someone’s health & care.